Myelin Sheath Damage Has Affected My Vagina Will I Ever Feel It Again
Introduction [edit | edit source]
Ofttimes, people who experience pelvic pain do non realize stress is highly correlated to their symptoms.[1] This is a outcome of the pelvic stress reflex response, in which the pelvic floor muscles actively contract in response to physical, or mental stress.[ane]
What Happens When the Body Is Under Stress? [edit | edit source]
Muscular Component - Pelvic Stress Reflex Response [edit | edit source]
The second layer of the pelvic floor includes the
- Urethral sphincter (sphincter urethrae)
- Compressor urethrae
- Sphincter urethral vaginalis
These muscular structures help command the menstruation of urine through the urethra.[2] There is a passive and active component to the contraction of the sphincters.[2] The passive component involves transmitting intra-abdominal pressure level to the urethra which mainly regulates the pressure at the neck of the bladder. The active component mainly controls the pressure distal to the bladder cervix, which is of import for urethral closure during stress conditions. The active component involves the reflexive contraction of external sphincter muscles. Thus, physical stress volition increase the contraction via the pelvic stress reflex response which can lead to tightness and weakness of the pelvic floor muscles.[2]
Hormonal Component – HPA Axis and Cortisol [edit | edit source]
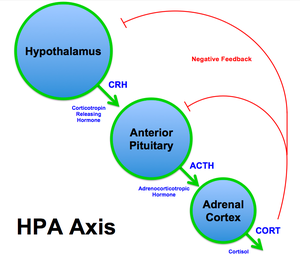
Response of HPA axis to stressors
HPA Axis [edit | edit source]
When the body identifies a stressor, it responds via the hypothalamic-pituitary-adrenal (HPA) axis.[3] This is a feedback system that maintains various body systems such as digestion, immune role, mood, energy and sexual practice.[3] Upon exposure to stress, the trunk perceives it using the hypothalamus which then releases corticotropin-releasing hormone (CRH).[iii] CRH and then triggers the pituitary gland to release adrenocorticotrophic hormone (ACTH) and finally signals the adrenal gland to release epinephrine (or adrenaline), norepinephrine and cortisol.[3]
Epinephrine and norepinephrine are released immediately after the body senses a stressor and these hormones break down just as fast.[iii] In contrast, cortisol is released about 10 minutes after the stressor is detected and tin can circulate in the trunk for almost one to two hours afterward.[iii]
Role of cortisol and immune function [edit | edit source]
I) Cortisol [edit | edit source]
- Normal levels (short-term effects): Cortisol is understood as the stress hormone of the body. Levels of cortisol vary throughout the twenty-four hour period, increasing in the morning to help wake upward the body and decreasing as the twenty-four hours passes.[ane] Cortisol levels follow the torso'due south circadian rhythm which helps immune functions such as prison cell repair.[1] Symptoms of loftier cortisol levels can include feet, agitation, poor sleep, 'wired merely tired' feeling and a fast pulse.[one]
- Abnormal levels (long-term furnishings): When the body is under stressful conditions, constant activation of the HPA centrality may occur.[1] The adrenal glands release high levels of cortisol which accumulate in the body.[1] Abiding stressors demands a constant release of cortisol, thus depleting the body of nutrients needed to produce the hormone. Exhaustion occurs when the body is not capable of producing more cortisol which compromises immune function likewise every bit increasing symptoms of pain, slower wound healing, decreased ability to handle smaller stressors, emotional issues and poor sleep.[1]
II) Impact of depression cortisol levels on pelvic pain [edit | edit source]
In numerous atmospheric condition related to pelvic pain, cortisol levels are lower than usual because the body has reached the burnout phase.[i] Long-term stressors have demanded the body to produce increased levels of cortisol for a prolonged time and now the body is depleted of nutrients to produce cortisol.[1]
- Endometriosis: The amount of cortisol released to help wake up in the morning was lower amidst women with endometriosis compared to command groups.[4] In fact, at that place were overall lower levels of cortisol in the endometriosis group. As well, women who reported intense pain with sexual practice and women experiencing infertility had lower cortisol levels than control groups.[4]
- Interstitial Cystitis (IC): Women with IC which lower amounts of cortisol in the morning also had a college rate of nocturnal urinary frequency (nocturia).[5] In add-on, they were likely to have greater pain in the lower belly every bit the bladder became full with fluid likewise as an increase in nocturia and frequency of urination throughout the mean solar day.[5]
- Vulvovaginal Candidiasis (vaginal yeast infection): Women who experienced repeated cases of yeast infections had a lower increase in cortisol in the morning and throughout the day compared to controls.[3]
- Vulvodynia: Women with vulvodynia had lower levels of cortisol in the morning and also had more symptoms of stress compared to control groups.[3]
Stress Tin Lead to Nonrelaxing Pelvic Floor Dysfunction (NPFD) [edit | edit source]
Information technology is more ordinarily understood that diverse pelvic flooring disorders are due to over-relaxed muscles (e.g. pelvic organ prolapse or urinary stress incontinence). This increases the likelihood that these disorders can exist identified and individuals tin can begin appropriate treatment.[6] In contrast, NPFD is not as easily identified considering individuals tin can present with a wide range of nonspecific symptoms including hurting, sexual dysfunction as well every bit problems with defecation or urination. This presentation may point that the pelvic flooring muscles and urinary and anal sphincters require relaxation and co-ordination rather than tightening. These symptoms are likely to have negative touch on the quality of life thus clinicians tin can use psycho-social questionnaires to assess the variety of stressors that may be impacting the patient's pelvic health.[half-dozen] Interventions can focus on managing stressors, such every bit patient education to help adopt good for you habits to command stress levels, or referring to individual to seeking further counselling if indicated past the questionnaires.[6]
Treatment Options [edit | edit source]
Physiotherapy [edit | edit source]
Increasing cortisol levels [edit | edit source]
It is evident that individuals with pelvic pain have factors that disrupt the usual cortisol cycle.[4] The combined event of physiotherapy and psychotherapy treatments in women with chronic pelvic pain can assistance to increase cortisol levels after handling and attain similar levels of cortisol as women without symptoms. Pelvic floor physiotherapists (PTs) can perform external and internal exams of the belly and pelvic area to assess if the muscles are weak or tight and administrate appropriate treatment. If the muscles are weak, PTs tin can teach exercises to strengthen the pelvic flooring. If the muscles are tight, PTs can perform internal releases of the pelvic floor muscles to help relieve the tension in the muscle and prescribe exercises to promote normal motor patterns in the muscles. Please run into this Physiopedia article for more than information to how physiotherapy tin be the solution to addressing pelvic hurting.
Relaxation, beingness mindful of pelvic floor [edit | edit source]
The PT tin utilize various strategies to increment awareness of the pelvic flooring muscles in guild to help the patient build self-management skills to cope with stress and contributing factors to NPFD.[6] The key is to introduce strategies early as possible, efficiently and effectively, past identifying the wide range of factors that tin lead to NPFD. Strategies include patient teaching about factors that influence the construction and function of the pelvic floor and conducting tests to confirm a diagnosis. The PT and patient can collaboratively develop appropriate goals to address the cause of pelvic pain and increment their quality of life.[6]
Naturopathy [edit | edit source]
Naturopathic doctors can address NPFD by examining the 'whole picture' and trying to identify the cause of the problem.[7] If long-term stressors are over-producing cortisol leading to the depletion of nutrients, then the trunk lacks specific nutrients for healthy performance adrenal glands. The naturopath may recommend taking specific vitamins or supplements which tin increase the production of cortisol.[7]
References [edit | edit source]
- ↑ 1.0 1.1 1.2 ane.3 i.iv one.5 1.6 i.7 1.8 ane.ix Stephens MA, Wand G. Stress and the HPA axis: Role of glucocorticoids in alcohol dependence. Alcohol inquiry: current reviews. 2012.
- ↑ ii.0 2.1 two.2 Thüroff JW, Casper F, Heidler H. Pelvic floor stress response: reflex contraction with pressure transmission to the urethra. Investigative Urology ii 1987 (pp. 124-130). Springer, Berlin, Heidelberg. Available from: https://link.springer.com/chapter/x.1007/978-3-642-72735-1_19
- ↑ 3.0 3.1 3.2 3.3 3.iv 3.five 3.half-dozen three.vii Petrelluzzi One thousand, Garcia 1000, Petta C, Grassi-Kassisse D, Spadari-Bratfisch R. Salivary cortisol concentrations, stress and quality of life in women with endometriosis and chronic pelvic pain.Stress. 2008;11(v):390-397. doi:10.1080/10253890701840610.
- ↑ four.0 four.one 4.2 Friggi Sebe Petrelluzzi Yard, Garcia Thou, Petta C et al. Concrete therapy and psychological intervention normalize cortisol levels and amend vitality in women with endometriosis.Journal of Psychosomatic Obstetrics & Gynecology. 2012;33(4):191-198. doi:10.3109/0167482x.2012.729625.
- ↑ 5.0 5.i Schrepf A, O'Donnell Yard, Luo Y, Bradley C, Kreder Thou, Lutgendorf S. Inflammation and Symptom Change in Interstitial Cystitis or Float Pain Syndrome: A Multidisciplinary Arroyo to the Study of Chronic Pelvic Pain Research Network Report.Urology. 2016;90:56-61. doi:ten.1016/j.urology.2015.12.040.
- ↑ half-dozen.0 6.i six.2 half-dozen.3 six.4 Faubion SS, Shuster LT, Bharucha AE. Recognition and management of nonrelaxing pelvic flooring dysfunction. InMayo Clinic Proceedings 2012 Feb one (Vol. 87, No. 2, pp. 187-193). Elsevier. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3498251/pdf/main.pdf
- ↑ 7.0 seven.1 Priolo, A. Stress, Cortisol and Pelvic Pain. 2018. Retrieved from https://www.proactiveph.com/blog/2018/05/16/stress-cortisol-and-pelvic-pain.html
thompsonfreat1962.blogspot.com
Source: https://www.physio-pedia.com/Impact_of_stress_and_cortisol_levels_on_pelvic_pain_and_pelvic_stress_reflex_response
0 Response to "Myelin Sheath Damage Has Affected My Vagina Will I Ever Feel It Again"
Post a Comment